Huntington’s disease remains without a cure in 2025. Clinical practice focuses on symptom control while a new wave of molecular programmes seeks to slow or halt neurodegeneration. The evidence base points in one direction. Approved drugs manage manifestations such as chorea and psychiatric symptoms. Investigational therapies that target the mutant huntingtin pathway aim for disease modification rather than reversal. In parallel, artificial intelligence is reshaping trial design, endpoint sensitivity, and regulatory strategy. This convergence of advanced biology and computational methods has shifted expectations about what meaningful progress looks like. The question facing researchers and professionals is not whether a cure exists. It is how fast validated disease modification can be delivered under frameworks that protect patients and preserve evidential standards. The following analysis sets out clear definitions, weighs current standards of care, profiles late-stage pipelines, tracks biomarker maturity, details AI contributions, and explains the regulatory context that now governs both software and advanced therapy medicinal products.
Defining cure, disease modification and symptomatic care in Huntington’s disease
Precision in terminology is essential. A cure would eradicate the pathogenic process and restore function without ongoing treatment. A disease-modifying therapy would slow or halt underlying neurodegeneration with effects shown on validated clinical outcomes or on surrogate measures considered reasonably likely to predict clinical benefit. A symptomatic treatment improves specific features such as chorea, mood change, or irritability without altering progression. These definitions shape trial endpoints, patient expectations, and the stringency of regulatory review. They also prevent category drift, in which symptomatic benefit is overinterpreted as modification of the disease course. By holding to this framework, claims can be adjudicated against consistent standards that align with national guidance and established regulatory language.
The 2025 verdict confirms no cure and a symptomatic standard of care
The evidence is unambiguous. There is no curative therapy for Huntington’s disease as of August 2025. Available medicines target symptoms and do not reverse neuronal loss or restore function after discontinuation. Late-stage programmes are designed to test disease modification. None seeks full reversal of established pathology. Public health authorities consistently describe care as supportive with symptom control and multidisciplinary management. The research frontier is now concentrated on therapeutic strategies that lower huntingtin production or activity and on study designs capable of detecting modest but meaningful slowing of decline.
A landmark signal emerges
On 24 September 2025, a BBC report described trial results from uniQure’s AMT-130 programme showing a 75% slowing of clinical progression over three years following neurosurgical gene therapy. Professors Sarah Tabrizi and Ed Wild, who led the UK arm, characterised the outcome as “spectacular” and potentially life-changing. Patients maintained function well beyond expected trajectories, with some returning to work or walking when wheelchair use had been anticipated. The company intends to submit for US licensing in the first quarter of 2026.
These results do not alter the 2025 verdict that no therapy has yet achieved regulatory approval or established a cure. However, they do represent the first credible demonstration of disease modification at a magnitude that may translate into decades of quality life. The data are not yet peer-reviewed and come from a small sample, so interpretation must remain cautious. Even so, the trial marks a turning point: Huntington’s disease is now moving from theoretical disease modification towards tangible clinical impact.

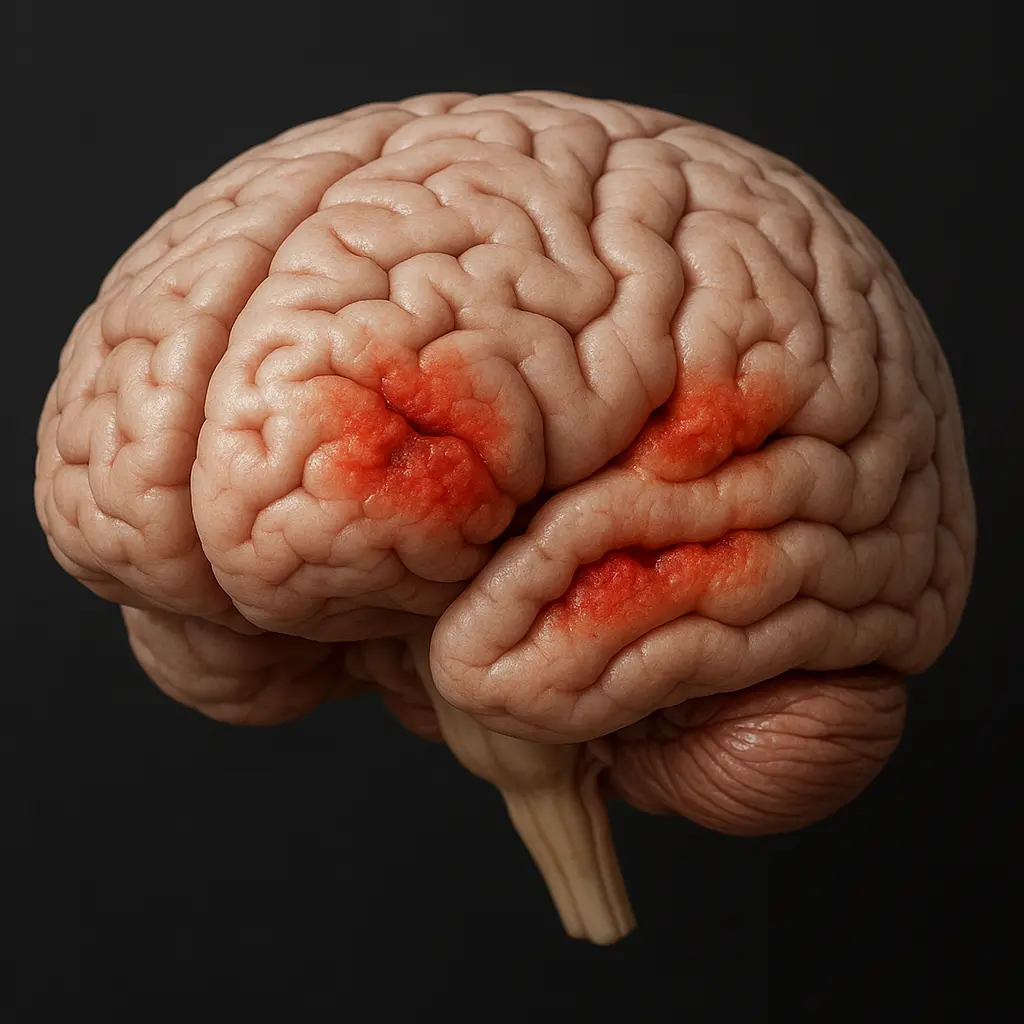
Symptomatic management focuses on chorea and psychiatric features
Treatment remains centred on improving daily function and quality of life. The clearest progress concerns hyperkinetic movement control using VMAT2 inhibitors. Tetrabenazine provided the initial proof of efficacy with a clinically relevant reduction on chorea ratings, although dosing is constrained by sedation, parkinsonism, akathisia, and a boxed warning for depression and suicidality that mandates careful monitoring. Deutetrabenazine uses deuteration to extend metabolite half-life and support twice-daily administration at lower total doses. In the first HD study, deutetrabenazine achieved a significant improvement in the Total Maximal Chorea score with durable benefit in extension follow-up and a safety profile that remained manageable at higher exposures. Valbenazine extended the class by offering once daily dosing and a positive pivotal readout on the same chorea metric with an exposure range validated by population modelling. All agents carry warnings regarding mood and suicidality risk.
Psychiatric management follows general principles, with SSRIs often used for depression and irritability and atypical antipsychotics reserved for psychosis or severe behavioural disturbance. Cognitive impairment lacks proven pharmacological treatment. Structured allied health support remains central. These realities underscore why disease modification is the leading research priority.
Real fact: Valbenazine became the third VMAT2 inhibitor approved in the United States for Huntington’s disease chorea in August 2023 and introduced once daily dosing convenience.
Huntingtin-lowering pipelines advance across ASO RNA interference, splicing and gene therapy
Therapeutic innovation is now anchored to the genetic cause of the disease. Multiple modalities pursue the reduction of the toxic protein produced by the expanded CAG repeat. Antisense oligonucleotides administered intrathecally recruit RNase H to degrade target transcripts. RNA interference delivered to the central nervous system engages the RISC complex to silence messenger RNA. Small molecules taken orally can alter pre-messenger RNA splicing to induce degradation. AAV-based gene therapy can deliver a DNA cassette that expresses an artificial microRNA for long-term suppression. Across these approaches, the shared goal is a sustained reduction of mutant huntingtin within the brain at levels that preserve safety margins for wild-type function.
Tominersen development resets dosing expectations and patient selection
Tominersen is a non-selective antisense oligonucleotide that lowers total huntingtin. The GENERATION HD1 Phase 3 study stopped early in 2021 on the advice of an independent data monitoring committee after an unfavourable benefit-to-risk profile emerged. There was no clinical benefit on the composite Unified Huntington’s Disease Rating Scale, and outcomes worsened in the more frequent dosing arm every 8 weeks compared with both placebo and the every 16 weeks arm. Ventricular enlargement increased more in the frequent dosing group, raising safety concerns linked to dosing intensity. The field took two critical lessons. First, more suppression is not always better. A narrow therapeutic window likely exists in which excessive total lowering may impair essential functions of wild-type huntingtin or reflect chemistry-related toxicity. Second, earlier intervention may matter. Post hoc analyses suggested a possible signal in younger adults with lower disease burden. Roche therefore launched GENERATION HD2 to evaluate dosing every 16 weeks at 60 mg and 100 mg. In April 2025, following another monitoring review, the 60 mg arm was discontinued, and participants moved to 100 mg based on a higher probability of benefit and unchanged safety findings. The study is planned to be read out in 2026.
AMT 130 gene therapy signals biomarker change and sets a new regulatory path
AMT 130 is a one-time AAV5 delivered therapy that uses neurosurgical administration into the caudate and putamen to express an artificial microRNA that lowers total huntingtin. United States and European trials have evaluated low and high doses in early manifest disease. As the follow-up has been extended to 24 months, safety has remained acceptable, and biomarkers have moved in a favourable direction. Cerebrospinal fluid neurofilament light fell significantly on average across cohorts, consistent with reduced ongoing neuronal injury. Exploratory analyses suggest stabilisation trends on composite clinical scores and motor ratings compared with an external control group derived from Enrol HD natural history data.
The regulatory strategy is notable. The programme holds Fast Track, Orphan Drug, Regenerative Medicine Advanced Therapy, and Breakthrough Therapy designations. After formal engagement with the United States regulator, agreement was reached to pursue Accelerated Approval using composite clinical outcomes supported by neurofilament light reduction as a surrogate considered reasonably likely to predict benefit. The pivotal evidence can come from the ongoing Phase 1 and 2 experience using Enrol HD as a well-characterised external comparator, avoiding a significant pre-approval Phase 3 randomised trial. A biologics licence application is planned for the first quarter of 2026. If accepted, this pathway could bring the first disease-modifying therapy to patients years sooner and create a template for other neurodegenerative indications.
PTC518, as an oral splicing modulator, shows pharmacodynamic and clinical signals
PTC518, also called votoplam, is an orally available small molecule that modifies huntingtin pre-messenger RNA splicing to insert a premature stop signal and drive transcript degradation. The practicality of an oral regimen is high because it removes the need for repeated lumbar punctures or neurosurgery and broadens access across neurology services. A global collaboration with Novartis announced in late 2024 underscored confidence in the approach. In the PIVOT HD Phase 2 study of Stage 2 and 3 disease, dose-dependent lowering of blood huntingtin was highly significant at 12 weeks. At 12 months, the 10 mg dose achieved a 39% reduction of blood huntingtin in Stage 2 participants. In those with 24 months of exposure, plasma neurofilament light fell by 14% from baseline at 10 mg, and trends moved in a favourable direction on the composite clinical scale relative to matched natural history. Safety and tolerability remained acceptable, and no treatment-related spikes in neurofilament light were observed. The combined pharmacodynamic and clinical signals mark this as one of the most pragmatic avenues to scalable disease modification.
Allele selective WVE 003 links target engagement with caudate atrophy
WVE 003 is an allele-selective antisense oligonucleotide that exploits a common single-nucleotide polymorphism called SNP3 to preferentially lower mutant huntingtin in about 40% of the patient population while preserving wild-type protein. In SELECT HD, multi-dose administration of 30 mg every 8 weeks reduced cerebrospinal fluid mutant huntingtin by a mean of 46% compared with placebo at 24 weeks, with effects that persisted beyond the final dose. Levels of wild-type huntingtin were maintained as intended. Safety was favourable with no serious adverse events reported. The most critical observation linked biology to structure. Greater mutant huntingtin reduction correlated with slower caudate volume loss measured by MRI with r equal to minus 0.50 and p equal to 0.047. This is the first clinical evidence connecting allele-selective target engagement to a downstream imaging marker central to the disease. The sponsor is discussing an Accelerated Approval strategy that uses caudate atrophy as a surrogate endpoint and has secured United States Orphan Drug status. A pivotal Phase 2 and 3 programme is planned to begin in the second half of 2025.
ALN HTT02 explores exon one targeting with RNA interference
ALN HTT02 is an RNA interference therapy for intrathecal delivery that targets exon 1 of the huntingtin transcript. Exon 1 encodes the expanded polyglutamine fragment thought to be a key toxic species. A single ascending dose Phase 1 study was launched in late 2024, involving up to 54 adults in Stage 2 or early Stage 3. The trial is enrolling, and initial pharmacokinetic and pharmacodynamic results are anticipated in 2026. This differentiated focus on exon 1 aligns with mechanistic work that implicates N-terminal fragments in early pathobiology and may complement programmes that reduce total protein.
Biomarkers and endpoints evolve to enable sensitive and reliable assessment
The field has shifted from single domain scales to composite outcomes and biologically grounded measures. The composite Unified Huntington’s Disease Rating Scale, known as cUHDRS, combines functional capacity, motor performance, and two cognitive tests into a single metric that detects change in early manifest disease with strong reliability. A change of about 1.2 points over a year is clinically essential. Placebo effects can be pronounced, especially in motor and cognitive components, which complicates interpretation and drives interest in objective measures.
Neurofilament light is now the leading fluid biomarker. It is a structural axonal protein that rises in the central fluid and blood during neuronal injury. Plasma levels are elevated years before predicted onset, increase with stage, and correlate closely with cerebrospinal fluid concentrations, with r equal to 0.868. Baseline plasma values predict timing of clinical conversion and subsequent rates of cognitive decline and atrophy. The rate of change accelerates with progression. Trials now use neurofilament light routinely for pharmacodynamic readouts and monitoring, and reductions are taken as strong evidence of an effect on neurodegeneration.
Imaging endpoints have advanced from supportive to potentially regulatory. Caudate volume loss measured by volumetric MRI tracks the core neuropathology of striatal atrophy and correlates with clinical decline across domains. The SELECT HD finding that larger reductions in mutant huntingtin align with slower caudate atrophy has elevated this measure to a candidate surrogate for Accelerated Approval discussions.
Digital measures have matured. The Huntington’s Disease Digital Motor Score aggregates smartphone sensor data from brief at home tasks, including balance, gait, and tapping. Reliability is excellent with an intraclass correlation coefficient above 0.95. Correlation with cUHDRS is moderate, with r equal to minus 0.5. Sensitivity to change is roughly double that of cUHDRS. This increase in signal can cut the required sample size by large margins or shorten the study duration while reducing participant burden and site variability. Validation under software as a medical device frameworks remains a prerequisite for pivotal use.
AI strengthens trial design endpoints and imaging analysis in Huntington’s disease
Machine learning now informs study planning and conduct at scale. Predictive models trained on Enroll HD data from more than twenty thousand participants can forecast individual trajectories far better than age and repeat length models. Sponsors use these forecasts to enrich for participants likely to progress within the trial window, improving power without inflating cohort size. The same models support synthetic control construction by generating counterfactual trajectories that complement or replace placebo groups. This approach underpins the external comparator strategy for AMT 130.
Digital endpoints depend on AI for feature extraction and scoring. The Huntington’s Disease Digital Motor Score uses algorithms to transform raw smartphone signals into a validated composite that captures change with high sensitivity. Imaging analysis has also been standardised. Automated pipelines using deep learning segment striatal structures across thousands of scans with high reproducibility. A harmonisation effort reanalysing historical datasets is building a large, consistent reference that reduces inter-rater variability and enables precise mapping of staging thresholds for the HD Integrated Staging System. These tools improve data quality and support qualification of imaging measures for regulatory decision making.
Regulatory frameworks for AI and advanced therapies define parallel pathways
Regulation has adapted to software and advanced biologics. In the United States, AI-enabled software functions used for medical purposes are regulated as software as a medical device. Draft guidance issued in January 2025 emphasises a total product lifecycle approach that documents design, validation, data governance, and cybersecurity. Developers can include a predetermined change control plan that specifies future model updates and validation steps. Approval of that plan allows updates without new submissions, which is essential for adaptive algorithms. For drug sponsors, this creates parallel pathways. A company that relies on a novel digital endpoint must secure clearance or authorisation for the device while also obtaining drug approval for the therapy. New competencies in software engineering, data science, and human factors are now part of development operations.
In Europe, the medicines regulator, in collaboration with national agencies, has set a risk-based, human-centric framework for AI in the medicinal product lifecycle. Tools that influence primary endpoints are considered high risk and high impact. They require detailed evidence on training data, validation methods, performance metrics, and interpretability. Sound Clinical Practice principles apply, including pre-specification before unblinding for fixed algorithms. A first qualification opinion on an AI methodology in March 2025 signals willingness to accept AI-generated evidence when validation is robust and traceable. For gene therapy and other advanced therapy products, expedited tools exist but still require rigorous demonstration of quality, safety, and efficacy.
Risks and lessons guide the next wave of Huntington’s disease development
Programmes that lower huntingtin face two broad categories of risk. First is the role of wild-type huntingtin. The protein supports axonal transport and neuronal health, including the movement of brain-derived neurotrophic factor. Non-selective lowering could harm these functions if suppression is excessive or prolonged. The tominersen experience reinforced this concern and strengthened the case for allele selective strategies such as WVE 003 that spare wild type protein. Second are delivery and off-target issues. Intrathecal administration is invasive and can be associated with procedure-related events. High concentrations of some antisense chemistries have triggered transient neurotoxicity in preclinical settings. Neurosurgical delivery for gene therapy has its own risk profile. Hybridisation-dependent off-target binding is a known risk for nucleic acid therapeutics that can be mitigated through careful design and screening.
The discontinuation of GENERATION HD1 yielded practical guidance. Dose and frequency must be optimised rather than maximised. Dosing every 16 weeks appears safer than every 8 weeks for this chemistry. Patient selection likely matters. Younger adults with lower disease burden may derive more benefit because less irreversible pathology is present. Ventricular volume has emerged as a safety biomarker that should be tracked whenever intrathecal antisense agents are used, given the observed expansion under more intensive dosing. These lessons have been integrated into current protocols and inform both monitoring and inclusion criteria.
Conclusion provides a clear outlook for disease modification and trial efficiency
The state of play in 2025 is defined by clarity and momentum. There is no cure for Huntington’s disease. Symptomatic care, especially with VMAT2 inhibitors, improves function and reduces distressing movements but does not alter progression. At the same time, the leading candidates for first-generation disease modification now combine three strengths. They show target engagement in people. They move validated biomarkers in the right direction, including neurofilament light and caudate volume. They have a credible regulatory path that may include Accelerated Approval supported by external controls and surrogate endpoints.
AI is an essential accelerator rather than a speculative add-on. Predictive models enhance enrolment and reduce reliance on placebo. Digital biomarkers raise sensitivity and lower burden. Automated imaging enables harmonised, large-scale analyses. Regulators have put forward frameworks that can accommodate these tools without compromising safety or evidential standards. The following two years will test whether this integrated approach can deliver the first therapy that slows the course of the disease in routine practice. Think of the field as a vessel leaving harbour with better charts, a sturdier hull, and steadier navigation. The destination is not guaranteed, yet the route is mapped with more precision than at any previous point.








